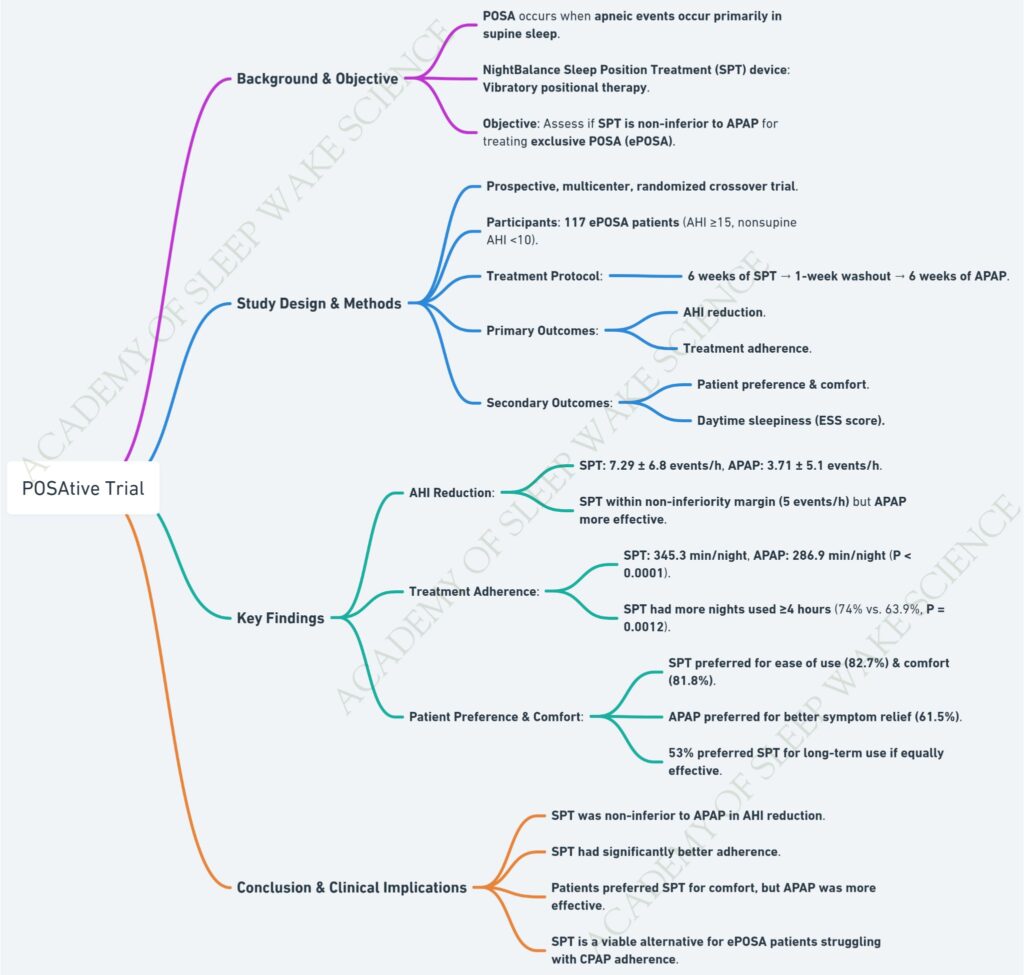
Comparative Analysis: SUPA OSA Trial vs. Singapore POSA Study vs. POSAtive Trial
| Parameter | SUPA OSA Trial | Singapore POSA Study | POSAtive Trial |
|---|---|---|---|
| Objective | Assess non-inferiority of supine alarm devices vs. CPAP in reducing daytime sleepiness | Assess non-inferiority of vibratory positional therapy (PT) device vs. CPAP in treating POSA | Assess non-inferiority of NightBalance Sleep Position Treatment (SPT) vs. APAP in treating ePOSA |
| Study Design | Crossover randomized controlled trial (RCT) | Crossover randomized controlled trial (RCT) | Prospective multicenter randomized crossover trial |
| Sample Size | 40 patients | 40 patients | 117 patients |
| Inclusion Criteria | Supine-isolated OSA, ESS ≥8 | POSA diagnosis with AHI >10, supine AHI ≥2× non-supine AHI, ESS ≥10 | ePOSA (AHI ≥15, nsAHI <10) |
| Intervention | Supine alarm device vs. CPAP (buzzpod) | Vibratory PT device vs. CPAP (Nightshift) | SPT vs. APAP (night balance) |
| Primary Outcome | Change in Epworth Sleepiness Scale (ESS) | Change in Epworth Sleepiness Scale (ESS) | AHI reduction and treatment adherence |
| AHI Reduction | CPAP more effective but PT significantly reduced supine AHI | CPAP more effective (AHI: 4.0 vs. 13.0 events/hour for PT, p=0.001) | APAP significantly better (AHI: 3.71 vs. 7.29 events/hour for SPT, p<0.001) |
| Sleep Efficiency | No significant difference | No significant difference | No significant difference |
| Adherence | PT adherence higher than CPAP (5.7 vs. 3.9 h/night) | Adherence varied: CPAP preferred initially, PT adherence higher when used after CPAP | SPT adherence significantly higher than APAP (345.3 vs. 286.9 min/night, p<0.0001) |
| Patient Preference | Higher preference for PT over CPAP | 60% preferred CPAP, 20% PT, 20% neither | 53% preferred SPT for long-term use if equally effective |
| Conclusion | Supine alarm devices are non-inferior to CPAP for reducing sleepiness and show better adherence | PT device did not meet non-inferiority criteria, CPAP remained preferred due to better symptom relief | SPT was non-inferior to APAP in AHI reduction within a 5 events/h margin and had better adherence |
| Clinical Implications | PT is a viable alternative for supine-isolated OSA patients, with better adherence | CPAP remains first-line for POSA, but PT may be considered for patients intolerant to CPAP | SPT is a viable alternative to APAP for ePOSA, especially for those struggling with CPAP adherence |
Key Takeaways:
- All three trials examined positional therapy alternatives to CPAP.
- SUPA OSA Trial found non-inferiority of supine alarms vs. CPAP for sleepiness reduction, whereas Singapore POSA Study did not meet non-inferiority criteria.
- POSAtive Trial demonstrated SPT had better adherence but slightly higher AHI compared to APAP.
- CPAP remains superior in AHI reduction in all studies, though PT improves adherence in select patients.
- Patient preference varies, with SUPA trial favoring PT, Singapore study favoring CPAP, and POSAtive trial showing a balanced preference.