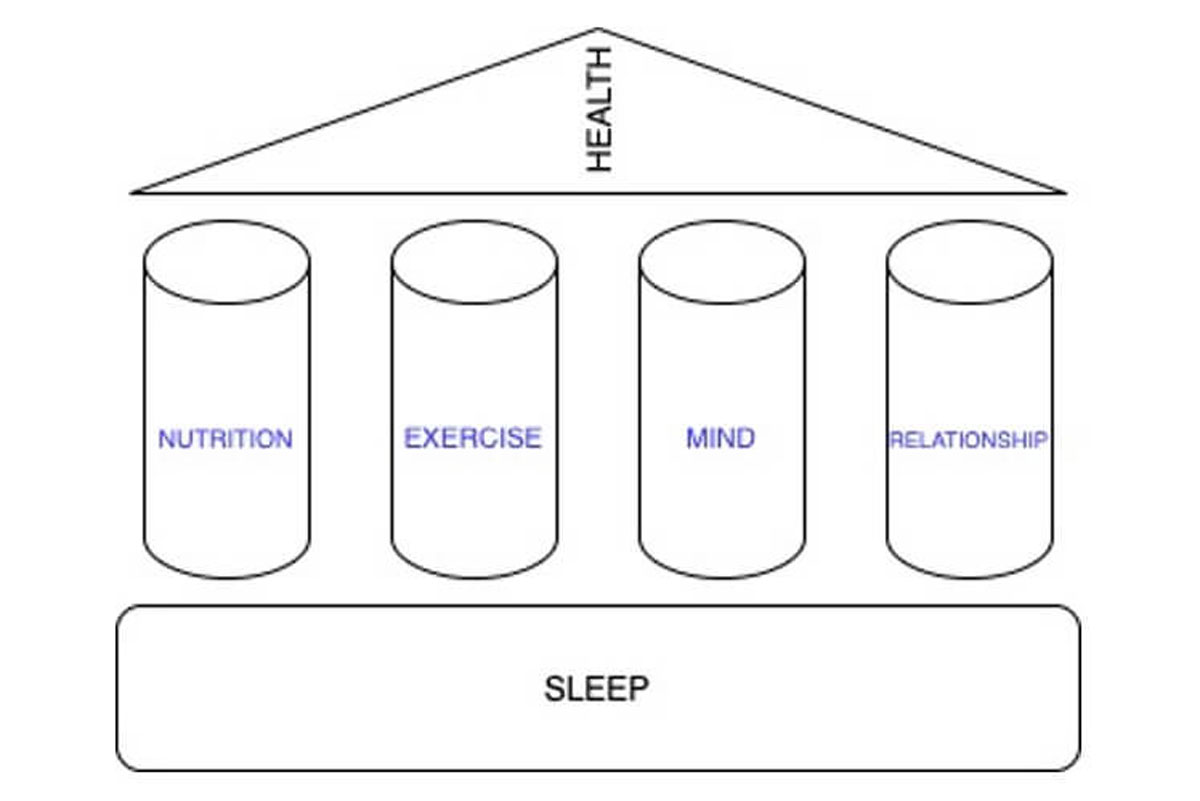
Now-a-days Sleep is defined as fifth pillar of health along with other four pillars- nutrition, exercise, mind/emotions and social/personal relationships. But I believe sleep is not fifth pillar, rather it is the foundation on which four pillars of nutrition, exercise, mind/emotions and social/personal relationships are standing to support good health.
For millions of years our ancestors have only moon light as the source of light at night. They will Sleep at night and during daytime go outside and get exposed to sunlight. Our ancestors had 12 hrs of day and 12hrs of darkness. The bodies adapted to this 12hrs day and darkness and developed certain rhythms, each rhythm following a particular time of the day or night eg: Sleep happening at night.
With the discovery of fire, our ancestors were exposed to artificial light at night for the first time which allowed them to be awake a little later into night as they could spend some time on cooking in a safe environment away from predators. This happened 300,000 years ago with daily usage of fire and probably made it possible to sleep on ground.1
In 19th century, Thomas Edison invented the bulb and changed our lives forever. Our homes and cities are now lit with bright light at night and work had been made possible 24hrs around the clock under well-lit conditions.
In 20th century, smart phones were invented. People often use these smart phones at night after getting into the bed and switching off the room lights. Now they get exposed to artificial light even in darkness after retiring to the bed, at a time when their bodies are looking forward to Sleeping.
Millions of years of evolution prepared our body to Sleep when the darkness sets in. There are physiological changes happening in our bodies with onset of darkness, which helps us to Sleep eg: Melatonin hormone is secreted with the onset of darkness which puts us to Sleep. Our ancestors had 7-9hrs of Sleep in 12hrs of darkness.
But in last 100-150 yrs we have decreased the duration of darkness and now we try to pack 7-9hrs of Sleep in 8-10hrs of darkness. Shift work made possible with a lot of technologies and most importantly well-lit conditions of our buildings, has even made us to pack 7-9hrs of Sleep during daytime with consequent health consequences.
This change in our behavior happened on a very small-time scale as far as evolution is concerned, which have not given enough time for our bodily functions to adapt to these lifestyle changes.
Light at night suppresses melatonin secretion and delays onset of Sleep.
Use of any type of screen- smart phone, tablet or computer- suppresses melatonin secretion and delays sleep onset because all these devices emit light with blue wavelength which suppresses melatonin secretion.2
Avoid reading ebooks on tablets at night as it has been shown that reading a story from an iPad decreased subjective sleepiness, delayed the EEG dynamics of slow wave activity by approximately 30 min.3
Reducing evening blue light advances sleep and melatonin.4 Use of Blue-light-blocking lenses (89-99,9% filter of blue light between 400-500 nm, general decrease of light intensity: 50%) 9hrs before switching off the lights advanced sleep and melatonin levels.4
Sleep is a universal phenomenon
Sleep is seen almost in all species on earth. Sleep must be serving some important function for our survival as the evolutionary process have not eliminated it during natural selection.
Sleep is a recurring state characterized by:
- Reduced awareness of and interaction with the external environment
- Reduced mobility and muscular activity
- Partial or complete cessation of voluntary behavior and awareness of self in the environment (reversible)
Types of Sleep:
There are two types of Sleep-
- Non rapid eye movement Sleep (NREM)
- Rapid eye movement Sleep (REM): Also called as dream Sleep
NREM Sleep have three substages-
- Stage N1
- Stage N2
- Stage N3: Also called as Deep sleep or slow wave sleep
A healthy person spends 75-80% of our sleep time in NREM and 20-25% of sleep time in REM Sleep every night.
Out of 75-80% of time in NREM sleep, we spend 3-8% of sleep time in Stage N1, 45-55% in Stage N2 and 15-20% in Stage N3 sleep.
We are awake for some time after we go to bed before we fall asleep. There is progression of sleep through cycles once we fall asleep.
Sleep cycle:
Sleep cycle is defined as progression of Sleep at night. A healthy adult enters first into NREM sleep and then REM sleep. Most of the healthy adults follow progression from Stage N1-Stage N2-Stage N3-Stage REM.
Stages N1, N2,N3 can vary in order of progression but it’s always NREM followed by REM sleep. Adult entering sleep via REM sleep may indicate sleep deprivation or an underlying Sleep disorder.
One episode of NREM followed by one episode of REM constitutes one Sleep cycle. There are 4-6 Sleep cycles in one night.
Timeline of Sleep to wake up events
One need to understand few concepts regarding what happens from the moment we go to bed until we wake up in the morning.
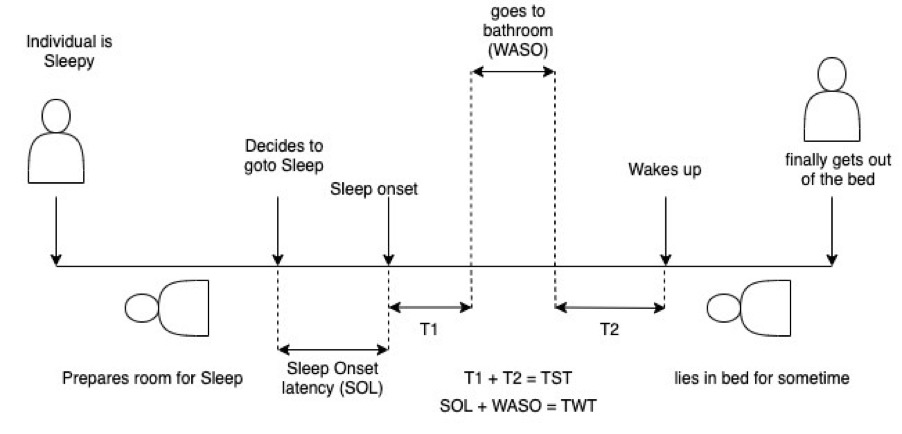
Fig: 1 Timeline of Sleep to wake up events. TST= Total Sleep Time, TWT= Total Wake Time, WASO= Wake after sleep onset.
Once a person is sleepy, they prepare the room for Sleep and then lie down in bed and switch of the lights.
Most of us take some time to fall asleep after lying down. This time from lying down to falling asleep is called “Sleep onset latency (SOL)”. For a healthy person SOL=10-20min. If SOL>30min, diagnosis of Sleep onset Insomnia is made.
Many people do not wake up at all after falling asleep and many wake up 0-1 times in the middle of the night. The time one spends awake after falling asleep is called “Wake after sleep onset (WASO)”. While awake, patient may just lie in bed or may go to bathroom to pass urine, drink water or may engage in any other activity. 0-1 awakenings of <5min are considered normal and WASO of <10min or 11-20min is considered normal.
The total time one spends asleep at night is called “Total Sleep Time (TST)”. We also calculate how much time was spent in bed. Total time spent in bed is referred to as “Time in Bed (TIB)”.
Ratio of TST/TIB gives an estimate of “Sleep Efficiency (SE)”. SE>95% OR 85-94% is considered normal
One wakes up in the morning, stays in bed for some time or gets out of the bed immediately and then is ready for the daily activities.
Defining good night Sleep
One should take care of three things for a good night Sleep-
- Sleep Regularity
- Sleep Duration
- Sleep Quality
- Attention to your chronotype
Sleep Regularity
Maintain a regular bed time and wake up time on weekdays as well as weekends.
Now-a-days people sleep less on weekdays due to work pressure or lifestyle changes and try to sleep more on weekends to make up for lost Sleep. When someone is sleeping less than what is required, they accumulate “Sleep debt” eg: if someone needs 7hrs Sleep per night and sleep only 6hrs, then the person is accumulating 1hr of Sleep debt per day.
Sleep debt has been defined as difference >60min between total sleep time required for the person and actual sleep hours obtained on weekdays. Severe sleep debt is difference >90min between total sleep time required for the person and actual sleep hours obtained on weekdays.5
The practice of sleeping more on weekend to make up for lost sleep on weekdays has been referred to as “Weekend Catch up Sleep”. Studies have shown that napping and weekend catch up sleep in adults compensated for severe sleep debt (>90min) only in 1 in 4 cases only.5
Sleep Duration
The total time one spends asleep at night is called “Total Sleep Time (TST)”. Each individuals Sleep requirements are different. Age specific guidelines on Sleep requirements have been published by National Sleep Foundation which can be referred for recommendations. It is summarized in Fig 2.
The first step to wake up fresh in the morning is to determine how much Sleep you need at night by working along with your Sleep Physician. Once you know the amount of Sleep you need, set your bed and wake up time accordingly.
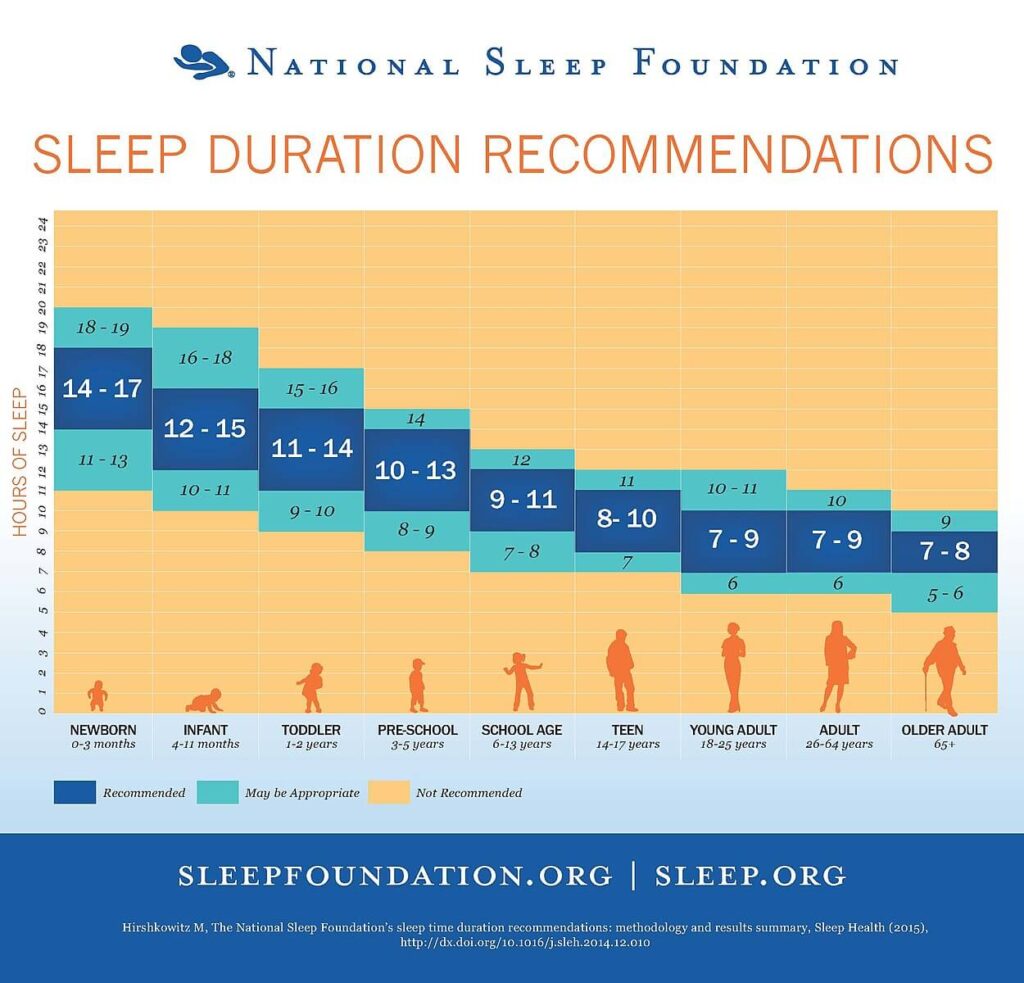
Fig 2: National Sleep Foundation TST recommendations for different age groups
Sleep quality
In the clinic we use following National Sleep Foundation defined indicators of good sleep quality to assess patients Sleep quality 6–
- Sleep Onset Latency (Good Sleep Quality= 0-30 min, Poor Sleep Quality= >45min)
- Number of awakenings >5 minutes (0-1)
- Wake after sleep onset (WASO) (<10min or 11-20min) and
- Sleep efficiency (>95% or 85-94%)
Many studies assess Sleep quality subjectively by asking one question “How was the quality of your sleep last night?” on a scale of 1 (very good) to 5 (very bad).7
If you are feeling refreshed upon awakening and did not need an alarm clock to wake you up, it is a good sign that you are getting both the quantity and quality that you need.
Pay attention to your Chronotype
Chronotype is defined as the internal circadian rhythm or body clock of an individual that influences the cycle of sleep and activity in a 24-hour period.
Traditionally three types of chronotypes have been proposed that prefer to Sleep and wake up at different times of the day.
- Morning type: Also called larks. These people prefer to wake up early in the morning and go to bed at around 10pm.
- Evening type: Also called night owls. They stay late up at night and wake up late in the morning.
- Neither
There are different ways to determine your chronotype-
- Using questionnaires like Horne-Ostberg questionnaire
- Measuring core body temperature and dim light melatonin onset
It is very important to know your chronotype as it will have an impact on your sleep. If your chronotype is night owl, you may face difficulty sleeping if you are trying to sleep at 10pm. If you are having difficulty in sleeping at night, I will advise to consult a Sleep physician who will not only determine your chronotype but also look into other potential causes of the sleep problem.
Recently a new way to profile chronotype shave been proposed. I feel this is will allow to include more people to be classified into different chronotypes as compared to traditional chronotyping. This chronotyping was proposed by Dr. Michael Breus. He proposes four types of chronotypes along with best timings for eating, exercising, coffee drinking and intimacy for each type-
- Bears:
- 50% people are bears.
- They are highly motivated, extroverted and bold people
- They are most productive from 9am-12pm
- Best time for them to sleep is 11pm-7am
- Best time for them to eat breakfast is 7:30am, lunch is 12:30pm and dinner 7:30pm
- Best time for the coffee to have maximum effect in morning is 9:30-11:30am
- Best time for them to run is 7:30am or 12:30pm
- Best time for intimacy is morning
- Lion:
- 15-20% people are Lions
- They are the leaders, athletic type, morning people
- They are most productive from 7am-12pm
- Best time for them to sleep is 9pm-5am
- Best time for them to eat breakfast is 6 am, lunch is 12 pm and dinner 6 pm
- Best time for the coffee to have maximum effect in morning is 8-10 am
- Best time for them to run is 5:30am
- Best time for intimacy is morning
- Wolves:
- 15-20% people are Wolves
- They are moody, introverted, creative and planners
- They are most productive from 10am-5pm
- Best time for them to sleep is 12am-8am
- Best time for them to eat breakfast is 8 am, lunch is 1 pm and dinner 8 pm
- Best time for the coffee to have maximum effect in morning is 12pm-2pm
- Best time for them to run is 6pm
- Best time for intimacy is morning
- Dolphins
- 10% of people are dolphins
- They are very intelligent, strive for perfection, introverted
- They are most productive throughout the day
- Best time for them to sleep varies and often suffer from Insomnia complaint
- Best time for them to eat breakfast is 8 am, lunch is 12 pm and dinner 7:30pm
- Best time for the coffee to have maximum effect in morning is 8:30-10am
- Best time for them to run is 7:30am
- Best time for intimacy is morning
Paying attention to your chronotype will allow you to choose the right timings for everything in your life and be in sync with your circadian rhythms to sleep well and lead a healthy life.
Benefits of good night Sleep
Sleep has been retained by evolution during the process of natural selection in almost all species on earth. An adult human being spends 1/3rd of their life time sleeping. Sleep cannot be an evolutionary mistake given we spend 1/3rd of our lives sleeping.
Some of the most plausible theories of benefits of good night Sleep are-
- Energy conservation: Basal metabolic rate (BMR) during sleep is lower than the BMR of awake state. It has been proposed that Sleep reduces caloric use and restores energy stores of the body which have been depleted during wakefulness.8
- Sleep restores brain energy stores: Studies have shown that in humans brain glucose consumption is approximately twice as high during waking as during slow wave sleep.9,10 This function is specific to NREM sleep as brain metabolic rate is higher during rapid eye movement sleep than during waking.11
- Sleep helps to have good immune function: We all know from our personal experiences that whenever we fall ill, we sleep more as sleep aids in recovery from the disease. Studies have shown that sleep or sleep loss influence immune function.12,13
Stage N3 sleep has been shown to play an important role in immunologic memory by consolidating immune response to infection.14
Sleep enhances the hepatitis A virus (HAV)-specific T helper (Th) cell response to vaccination.15
Shorter sleep duration on the two nights before the vaccination predicted fewer antibodies 1 and 4 months later.16
This information is very important in today’s world suffering from Corona pandemic and the ongoing vaccination drive against Corona virus. American academy of Sleep Medicine (AASM) recommends following before/after immunization for Corona virus for a good night Sleep- (https://aasm.org/healthy-sleep-and-immune-response-to-covid-19-vaccination/)
- Establish a bedtime and morning routine
- Ensure the bedroom is a space for sleep
- Set boundaries for blue light exposure
- Limit alcohol, caffeine and large meals before bedtime
- Sleep on it: try to get good sleep on the night after vaccination
I will suggest in addition to above recommendations, to get good night sleep 2 nights before the vaccination as well.
- Sleep helps to clear toxic metabolites from the brain: Study have shown that Short sleep duration (<6hrs) might be an early marker of Alzheimer disease.17 Alzheimer disease occurs due to accumulation of beta amyloid proteins in the brain.
There is a system called “Glymphatic system” in brain which helps to remove proteins linked to neurodegenerative diseases (β-amyloid, α-synuclein and tau).18 These proteins are present in the interstitial space surrounding cells of the brain. Glymphatic system consist of CSF recirculating through the brain interchanging with interstitial fluid (ISF) and helping to remove interstitial waste products and proteins, including β-amyloid.18 Glymphatic system activity is increased in Sleep as shown by Increased β-amyloid clearance during sleep.18
It has been shown that Slow wave sleep disruption increases beta amyloid levels acutely, and poorer sleep quality over several days increases tau protein levels.19
It looks like that maintaining sleep regularity, duration and quality may prevent onset of Alzheimer disease.
- Sleep helps in memory consolidation: Memory formation involves three physiological processes- Encoding, Consolidation and Recall. Sleep has been characterized as a brain state optimizing memory consolidation.20 Consolidation occurs during Slow wave sleep and transfer them for integration into the long term memory.20 Ensuing REM sleep may stabilize transformed memories.20
My advice is do not lose sleep before any exam. Study in time and Sleep well on the night of the examination.
- Sleep helps to regain our performance levels: We know that if we are tired and cannot perform a task, Sleep on it and try again next day. Studies have shown that after sleep deprivation performance is restored by sleep21 in a dose dependent manner.22
- Sleep is good for your cardiovascular health: The function of our heart and blood vessels is controlled by Autonomic nervous system (ANS). ANS have two divisions- Sympathetic nervous system and parasympathetic nervous system.
Sympathetic nervous system is stimulatory and increases contractility of heart, heart rate, cardiac output, increases metabolic demand of heart, increases blood pressure and cause blood vessel constriction.
Parasympathetic nervous system slows heart rate, decreases- contractility, cardiac output, metabolic demand, blood pressure and causes blood vessel relaxation.
The balance between sympathetic and parasympathetic nervous system maintains cardiovascular health.
During NREM Sleep (compared to Wake) there is a decrease in sympathetic activity and increase in parasympathetic activity.
During REM Sleep (Compared to NREM Sleep), there is decrease in sympathetic activity and increase in parasympathetic activity. Although, transient increase in Sympathetic activity happens during phasic REM Sleep.
During sleep, systolic blood pressure (BP) decreases by 10% as compared to wake systolic BP.23 This is called “Dipping BP” phenomenon23 which is positively correlated with %age of Stage N3 and negatively with WASO.24 Absence of the Dipping BP phenomenon is a predictor of adverse cardiovascular events in nonmedicated hypertensive patients.23
It has been shown that lower %age of Stage N3 sleep increases the risk of developing hypertension in future in both men and women.25
This data shows that Sleep is good for your cardiovascular health and my suggestion is- “Sleep well for a healthy heart”.
- Sleep improves athletic performance: It has been shown that there is a detrimental effect of sleep deprivation (a night or more without any sleep) and a beneficial effect of chronic sleep improvement (repeated exposure of strategies that improve sleep over weeks or months) on sports specific and physical performance.26-28 A consensus guideline29 has been published which suggest following for athletes Sleep to improve their performance-
- Provide Sleep education for athletes
- Screen athletes for Sleep problems
- Encourage naps if sleep opportunity is not enough
- Bank Sleep- Sleep extension prior to any major event
In this blog, I discussed about normal Sleep and its benefits. In my next blog I will discuss about how we can have a good night Sleep with 20tips on “Sleep hygiene” to help you Sleep better.
Until then “Sleep well. Sleep on time.”
References:
1. Wrangham R, Carmody R. Human adaptation to the control of fire. Evolutionary Anthropology: Issues, News, and Reviews. 2010;19(5):187-199.
2. Wahl S, Engelhardt M, Schaupp P, Lappe C, Ivanov IV. The inner clock-Blue light sets the human rhythm. J Biophotonics. 2019;12(12):e201900102.
3. Grønli J, Byrkjedal IK, Bjorvatn B, Nødtvedt Ø, Hamre B, Pallesen S. Reading from an iPad or from a book in bed: the impact on human sleep. A randomized controlled crossover trial. Sleep Med. 2016;21:86-92.
4. Zerbini G, Kantermann T, Merrow M. Strategies to decrease social jetlag: Reducing evening blue light advances sleep and melatonin. Eur J Neurosci. 2020;51(12):2355-2366.
5. Leger D, Richard JB, Collin O, Sauvet F, Faraut B. Napping and weekend catchup sleep do not fully compensate for high rates of sleep debt and short sleep at a population level (in a representative nationwide sample of 12,637 adults). Sleep Med. 2020;74:278-288.
6. Ohayon M, Wickwire EM, Hirshkowitz M, et al. National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health. 2017;3(1):6-19.
7. Brindle RC, Yu L, Buysse DJ, Hall MH. Empirical derivation of cutoff values for the sleep health metric and its relationship to cardiometabolic morbidity: results from the Midlife in the United States (MIDUS) study. Sleep. 2019;42(9).
8. Krueger JM, Frank MG, Wisor JP, Roy S. Sleep function: Toward elucidating an enigma. Sleep Med Rev. 2016;28:46-54.
9. Kennedy C, Gillin JC, Mendelson W, et al. Local cerebral glucose utilization in non-rapid eye movement sleep. Nature. 1982;297(5864):325-327.
10. Buchsbaum MS, Gillin JC, Wu J, et al. Regional cerebral glucose metabolic rate in human sleep assessed by positron emission tomography. Life Sciences. 1989;45(15):1349-1356.
11. Braun AR, Balkin TJ, Wesenten NJ, et al. Regional cerebral blood flow throughout the sleep-wake cycle. An H2(15)O PET study. Brain. 1997;120(7):1173-1197.
12. Imeri L, Opp MR. How (and why) the immune system makes us sleep. Nature Reviews Neuroscience. 2009;10(3):199-210.
13. Besedovsky L, Lange T, Born J. Sleep and immune function. Pflügers Archiv – European Journal of Physiology. 2012;463(1):121-137.
14. Besedovsky L, Lange T, Haack M. The Sleep-Immune Crosstalk in Health and Disease. Physiol Rev. 2019;99(3):1325-1380.
15. Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. 2012;463(1):121-137.
16. Prather AA, Pressman SD, Miller GE, Cohen S. Temporal Links Between Self-Reported Sleep and Antibody Responses to the Influenza Vaccine. International Journal of Behavioral Medicine. 2021;28(1):151-158.
17. Leng Y, Ackley SF, Glymour MM, Yaffe K, Brenowitz WD. Genetic Risk of Alzheimer’s Disease and Sleep Duration in Non-Demented Elders. Ann Neurol. 2021;89(1):177-181.
18. Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377.
19. Ju YS, Ooms SJ, Sutphen C, et al. Slow wave sleep disruption increases cerebrospinal fluid amyloid-β levels. Brain. 2017;140(8):2104-2111.
20. Rasch B, Born J. About sleep’s role in memory. Physiological reviews. 2013;93(2):681-766.
21. Rosa RR, Bonnet MH, Warm JS. Recovery of Performance During Sleep Following Sleep Deprivation. Psychophysiology. 1983;20(2):152-159.
22. Banks S, Van Dongen HPA, Maislin G, Dinges DF. Neurobehavioral Dynamics Following Chronic Sleep Restriction: Dose-Response Effects of One Night for Recovery. Sleep. 2010;33(8):1013-1026.
23. Bloomfield D, Park A. Night time blood pressure dip. World journal of cardiology. 2015;7(7):373-376.
24. Loredo JS, Nelesen R, Ancoli-Israel S, Dimsdale JE. Sleep quality and blood pressure dipping in normal adults. Sleep. 2004;27(6):1097-1103.
25. Javaheri S, Zhao YY, Punjabi NM, Quan SF, Gottlieb DJ, Redline S. Slow-Wave Sleep Is Associated With Incident Hypertension: The Sleep Heart Health Study. Sleep. 2018;41(1):zsx179.
26. Fullagar HH, Skorski S, Duffield R, Hammes D, Coutts AJ, Meyer T. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015;45(2):161-186.
27. Bonnar D, Bartel K, Kakoschke N, Lang C. Sleep Interventions Designed to Improve Athletic Performance and Recovery: A Systematic Review of Current Approaches. Sports Med. 2018;48(3):683-703.
28. Vitale KC, Owens R, Hopkins SR, Malhotra A. Sleep Hygiene for Optimizing Recovery in Athletes: Review and Recommendations. Int J Sports Med. 2019;40(8):535-543.
29. Walsh NP, Halson SL, Sargent C, et al. Sleep and the athlete: narrative review and 2021 expert consensus recommendations. Br J Sports Med. 2020.